https://www.valenzhealth.com/wp-content/uploads/2024/10/SOC-2-Web-Graphic-Test-6.png
432
600
Jessica Lahasky
https://www.valenzhealth.com/wp-content/uploads/2023/01/valenz-logo-1-23-3.png
Jessica Lahasky2024-10-10 18:22:022024-10-10 21:44:45Vālenz® Health Provider Credentialing Solution VPoint™ Attains SOC 2 Type II Certification for Strong Data Security
https://www.valenzhealth.com/wp-content/uploads/2024/10/SOC-2-Web-Graphic-Test-6.png
432
600
Jessica Lahasky
https://www.valenzhealth.com/wp-content/uploads/2023/01/valenz-logo-1-23-3.png
Jessica Lahasky2024-10-10 18:22:022024-10-10 21:44:45Vālenz® Health Provider Credentialing Solution VPoint™ Attains SOC 2 Type II Certification for Strong Data SecuritySimplify Your Health Plan Solutions With One Distinctly Different Partner
Valenz is the destination for group health employers, payers, providers and members to reduce costs, improve quality and elevate the healthcare experience.
Engaging Early and Often Across the Member Journey
Valenz integrates member-centric services with data-driven insights, connecting the dots with personalized service and guidance for high-quality care and improved outcomes.
1
2
3
4
5
6
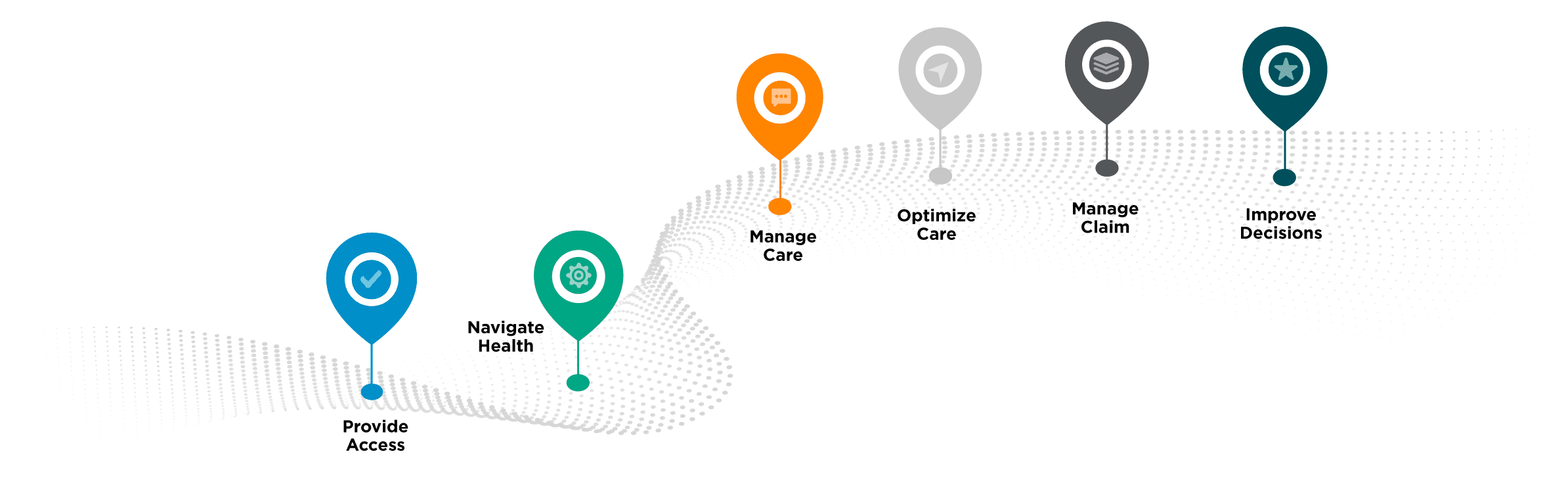
1
Member enrolls in the health plan.
Valenz delivers quality-first provider networks and reimbursement strategies with cost-saving, risk-reducing services to replace your high-cost contracted network plan – and you choose which network model will best serve your business and member needs.
2
Member seeks care services.
NaVcare provides intuitive member navigation, directing care to high-quality providers based on the member’s financial health and medical condition for better savings, outcomes and experiences, and referring to case management when needed.
3
Member is diagnosed and needs treatment.
Nurse-led care management targets the right care before services are rendered. Improve quality of care and maximize savings with personalized Case Management, Utilization Management and Disease Management.
4
Member needs close medical and pharmacy monitoring.
Accessing expansive cost and quality data sets, we optimize care with cost-effective pharmacy services, wraparound case management, and specialized and chronic care management for oncology, cardiology, diabetes, maternity and more.
5
Member’s claims are submitted for payment.
Protect payment integrity for your business and out-of-pocket costs for your members with our complete set of tools and services for systematic claim review, expert bill review with provider signoff, post-payment recovery services, claim and network repricing, and balance billing protection.
6
Member and health plan need costs to stop rising every year.
The Valenz platform to simplify healthcare leverages unparalleled data transparency and expansive analytics, aligning the summary plan description with cost-containment solutions for optimal stop loss underwriting to continuously optimize cost, quality and utilization for everyone.
Everyone Aligns on Our Platform to Win
Employers, payers, providers and value chain partners gain the efficiency and effectiveness they need to reduce healthcare spend.
Members enjoy greater access to care with lower out-of-pocket expense and improved health outcomes.
Group health employers transform their health insurance with Valenz, achieving greater savings, higher efficiency and exceptional member experiences.
Payers rely on Valenz data-driven solutions to reduce the trajectory of their healthcare costs.
Become a Valenz network partner and ensure high-quality care via our credential verification organization and compliance monitoring solutions.
We empower employees to make better, more informed health decisions and lead strong, vigorous and healthy lives.
Explore Case Studies and White Papers
See how we partnered with a collaborative of three schools representing 700+ members in deploying a fully integrated continuum of solutions to change the rising cost trajectory while improving the quality of care. The case study was independently reviewed and approved for accuracy by the Validation Institute.
Learn how Valenz V-Rated Solution identifies risks affecting the health plan, while aligning stop loss underwriting with the Summary Plan Description and cost containment solutions. V-Rated leverages alignment, balance, and transparency to bring back fiduciary responsibility and appropriate stop loss rating.
Capture the Power of the Platform to Simplify Healthcare
Connect with a team member today to learn how Valenz solutions can make a difference for you.